"DON’T WRITE OFF THE NHS"
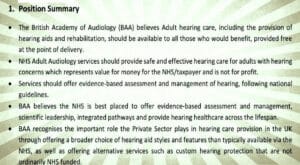
Foreseeable complexities surround proposals of a new shuffle of the old duality in hearing healthcare. The British Academy of Audiology has issued a position statement defending free audiology and the ability of the NHS to deliver services in the UK.

BAA leaders Samantha Lear (President) and Claire Benton (VP) talked to editor-in-chief Peter Wix on their organisation’s defence of standards, definitions, holistic services, and more qualities they see best safeguarded by the NHS. Their words reflect hope of persuading a new UK Government to galvanise NHS delivery, as well as fears that an intensifying debate may swing towards a policy chop-up of hearing care pathways.
The NHS can and should be the deliverer of audiology services in the UK, and free of charge to all who might benefit from them.
This is the essence of a new position statement issued by the largest association of UK professionals in hearing and balance, the British Academy of Audiology (BAA), which is the body most closely engaged with those working in hearing-related occupations in the NHS.
While it has the air of a manifesto, the paper – The Future of NHS Adult Hearing Loss Management does defend its advocacy with detailed and referenced reasoning, striving to show why and how ʺNHS Adult Audiology services should provide safe and effective hearing care for adultsʺ and that this can represent ʺvalue for money for the NHS/taxpayer and is not for profitʺ.
But it is the timing of this precise assertion of position that makes it more than headline tinder, coming within reflex pace of the opening thrusts of a campaign led by the retail group Specsavers, one currently gathering allies and interest across the audiology spectrum. Ultimately, as its presentation venues such as Westminster, Stormont, and the Senedd suggest, the ears the campaign most seeks to stimulate belong to policy makers.
The BAA’s position statement wants politicians to listen too. But the body’s President Sam Lear is keen for her group’s argument not to be framed as ʺprivate sector bad; NHS is goodʺ.
ʺOur statement is definitely not a reaction to the Specsavers one; we’re not interested in that tit-for-tat,ʺ says Lear despite the statement’s timing. Yet there is enough in both her words, and those of BAA VP, Claire Benton, to confirm the sense radiating from the position statement that this debate has the makings of a turning point for audiology in the UK, and that the scent of NHS blood is in the air. It may even point to wider implications in health.
ʺBAA aren’t anti private sector at all, and really see a role for both. But what we haven’t seen is governments investing in the NHS first and trying to make it work in the NHS first. It’s this: we don’t want to see a wholesale shift of the routine services as some quick fix for waiting lists,ʺ Lear spells out.
ʺWhat we want to see is consideration at local level. What is supposed to happen in England, particularly with ICSs [Integrated Care Systems], is that each region looks at what it needs and what it can deliver, and if there’s a region where use of the private sector to provide some NHS care is going to be the best thing we want to see it planned properly, so it’s joined up with local services.ʺ
This, maintains Lear, would avoid adults getting routine care in the private sector, then being ʺkicked outʺ after three years to return to NHS care. And she makes the BAA’s plea for not just proper planning but also funding so the NHS can try to make it work, ʺand trying to innovate, to see if it can be delivered properly within the NHS, where all the structures are there firstʺ.
Both President and VP echo the BAA position statement on the NHS having everything set up to deliver care and develop it into the future, crucially in prowess in governance, recent behind-the-scenes work in the UK pushing quality improvement programmes. The BAA sees the new statement as a way of supporting its members, reminding them that the infrastructure and governance are there for them to continue doing good work.
Can’t independent private practice chains provide similarly robust standards?
Lear answers carefully, but thinks they cannot be as holistic: ʺObviously they can match the training and the QA [Quality Assurance] for very specific parts of the pathway; the routine fitting… they can definitely do the training, and they could QA… But they haven’t got the whole governance infrastructure which most people don’t realise is there in the NHS, the whole department, the checks on your infection control, or your audit, or your language, or your patient information, or your links to refer to other departments… that whole wider government that the average person doesn’t even know exists. That doesn’t exist in the private sector; they might be able to tick off a box that they’re meeting specific QA standards for a procedure, but they can’t possibly have that all the other stuff.ʺ
Routine care…and hearing in total -“It can’t just be parcelled off”
One key current flowing through the position statement is the value of overall NHS care, a multidisciplinary approach and lifelong service that both BAA leaders passionately defend.
ʺHearing in total is being highlighted, so it’s not us, this is not a callback to any other report. This is our stance from BAA about investment in the NHS and the NHS delivery of hearing aids and care for adults with hearing loss,ʺ says soon-to-be (from November 2024 for two years) President Claire Benton.
BAA/graphic enhancement ANUK
ʺIt really undersells some adult hearing care by referring to it as routine and that it can just be parcelled off. I don’t think that’s respectful of those patients and what care they do need. It’s a very fine line, isn’t it, what someone would call routine and what someone would call complex and that’s not really being defined particularly well. I think what we’re trying to advocate for is to be mindful, not to just parcel off a group of patients and think that’s OK and that fixes it and the NHS will pick up the rest, because it doesn’t work like that,ʺ says Benton, before suggesting that the optics sphere provides evidence of patients not getting what they need: ʺPeople can’t afford the glasses that they may need. The more complex your eyesight is, the more expensive your lenses are, and therefore some people don’t buy them. And why should we not advocate to stop that for hearing?ʺ
The point is strongly echoed by current President Sam Lear, who stresses: ʺNo one person is routine. A person might be just pre-retirement age, fit into the criteria to to go off to the private sector, but actually that person will have a lot of needs, and without probing the particular situation, what meetings they are in, what are the illnesses, medical conditions they have, whether they have any sort of mental health issues around it, which could all be referred on in the NHS, it will just be looking at one specific part of them. It’s not holistic at all and that’s losing a lot.ʺ
ʺAn audiologist, even a fairly junior one, will have a lot of safeguarding training, a lot of sort of awareness of the patient as a whole person, and we’re very much moving towards more patient-centred care. You can’t divide it and just go ‘well,hearing, it’s routine’ and just look at a person’s ears. A patient that needs hearing aids isn’t just going to go down a three-year pathway and then be discharged; they’re with you for life and there is a concern as well that if there’s some sort of private contract to do that it will be a specific length of time and then they’ll be kicked out. What happens then? They go back in the NHS. So we just want a bit of honesty about this idea that we could take that bit out of the NHS and put it there and it’ll save the rest of the NHS and it will be good for patients. We need to know what we’re losing out as well,ʺ Lear underlines.
Is there a case for a primary care community audiology service?
IT’S TIME TO TALK ABOUT HEARING is a campaign launched by Specsavers in the form of a Hearing Health Report. It states that it is asking politicians and policy makers ʺto reduce pressure on GPs and other NHS hospital services by making more effective use of capacity and expertise that already exists in community services to extend NHS careʺ.
Unhappy with how this campaign is being worded, Claire Benton draws on her experience in NHS management: ʺI think we need to be really careful around language because community NHS provides. I provide 14 different community services around the Nottingham area so it’s not a new thing; a lot of NHS departments have a footprint.ʺ
Sam Lear backs this up: ʺThe language isn’t entirely honest because it’s not what most people would think of as primary care; it’s a different model. And as Claire said, NHS provides plenty of services in the community.ʺ
And it is not just the language of the proposal that the BAA chiefs oppose; Samantha Lear disputes the premise that the NHS would be helped by proposals the BAA sees as potentially ʺprivatising by stealthʺ.
ʺTo the average person,ʺ Lear argues, ʺa high street hearing aid shop might not be any more accessible than a hospital. It’s quite a ridiculous sort of twist. And also what I object to is that this is going to solve the problems that the NHS has. It’s not being entirely honest to the politicians it’s trying to sell to.ʺ
The BAA President also dismisses the argument that NHS resources could be freed up by taking routine care out of the equation, to leave many audiology services with more time resources. ʺThat is not what’s going to happen because we all know it’s the same workforce. There aren’t any extra audiologists, so those audiologists will be then working in the private sector, and a lot of the resourcing for those complex services comes from those big numbers they get for routine care. We just want politicians to realise it’s not the the fix that’s being sold to them. If anything, it’s going to exacerbate some of the problems.ʺ
The past bestows a poor image on the NHS in hearing care
Both the BAA President and VP argue that the hearing aids NHS patients receive are up to standard, but that their reputation is still tarnished by memories from the distant past, with the public still expecting ʺNHS beigeʺ.
ʺPeople play on that quite a lot, don’t they? And it doesn’t really represent what the NHS now offers for its technology. And people are drawn to the glamour of ‘Oh, I don’t want it to look NHS’ without really looking at what we do provide.ʺ Benton argues.
ʺWe could quite easily have flooded the supply chain with older devices that are cheaper, to help departments save money. But we don’t. We ensure that there’s a standard of hearing aid that’s available, and it all has to meet that basic standard. So we know that on supply chain, within the NHS, patients are being given pretty much up-to-date technology and the manufacturers are really narrowing that gap, some more than others, between what’s available privately, and you pay for a lot of cosmetics and really new technology. But the gap between when we get that on the NHS is really shrinking now and I think people underestimate what the devices that we can offer on the NHS actually do,ʺ continues Benton.

PW
Claire Benton, BAA VP: ″I think what we’re trying to advocate for is to be mindful, not to just parcel off a group of patients and think that’s OK and that fixes it and the NHS will pick up the rest, because it doesn’t work like that.″
The position statement does, however, concede BAA recognition of ʺthe important role the Private Sector plays in hearing care provision in the UK through offering a broader choice of hearing aid styles and features than typically available via the NHSʺ.
The question of technology differences between one device and another is balanced by Sam Lear: ʺYou can have the most fancy-schmancy hearing aid in the world, but if someone doesn’t take time to ask about that – patients need to try different features – fit it properly, do some sort of proper scientific testing, then it may as well be the most simple hearing aid,ʺ adding: ʺIf someone can afford that sort of care and they can go to an independent professional who really, really cares and spends a lot of time with their patient really asking about their lifestyle, what they want, and trying different features, that’s great! If someone can afford to and chooses to, that’s what they’re paying for, that bespoke stuff. But we’re not talking about that in this sort of private provision; we’re not talking about bespoke stuff, we’re talking about almost dumbing down the pathway, aren’t we?ʺ
Room for innovation in the NHS?
The BAA position statement places great emphasis on enabling change and diversity of working methods through liberating imagination and innovation: in service management, to tackle waiting lists, in technology and care models, in real estate use, and through removing barriers for the provision of remote care, through IT and information governance departments. Funding this is also called for, but how realistic is it in any sector to expect innovation?
ʺVery!,ʺ Benton asserts from her post as Head of Service at Nottingham University Hospitals NHS Trust (2018 to end of August 2024). ʺWe’ve just had a face-to-face Head-of-Service meeting and we had a variety of different people from services literally telling us what they have done, so it’s being delivered now, the innovation, to help cut waiting times down. They’re ensuring the quality. It’s been monitored appropriately. So all the checks are being done to make sure that it’s not just crashing through waiting lists to make people happy,ʺ continues Benton.
ʺSo it’s not that we’re waiting to find the innovation, it’s already happening. It’s just rolling that out and sharing that information more widely so everyone else can build that network to start using it.ʺ
Both Lear and Benton also back the NHS having the flexibility in structure and management set-up to foster such innovation.
A complex region-by-region panorama
But with the future of the UK’s hearing health pathways depending on policy directed by Government – and on properly funding that policy – how do these professionals leaders think things will evolve from this point of possible bifurcation?

PW
BAA President Sam Lear: ″Also what I object to is that this is going to solve the problems that the NHS has. It’s not being entirely honest to the politicians it’s trying to sell to.″
President Sam Lear is quick to point out that the situation cannot be reduced to a dual prospect: ʺIt’s not necessarily even two opposite things that can happen, because there are some regions where there isn’t the capacity in the NHS, and they’re likely going to have to have a coordinated server.ʺ
ʺIf a large chain company gets a contract to provide routine care in one area, and there’s a pathway in and out of the NHS, and it’s holistic and planned properly, that’s OK, we’re not going to be crying about that. But what we don’t want to see is what’s being proposed, ‘a national contract – there you go’, because we don’t think that’s good for patients or for NHS services. We think it will have eventually quite a detrimental effect,ʺ determines Lear.
Benson expands on the need to embrace the complexity of the situation: ʺPart of the good work that was being shared at Heads of Service [meetings] is how one area has worked really well with the independent sector and set up an Any Qualified Provider system that everyone is happy with, and that works, that’s got shared procurement.ʺ
ʺWe can work together. Like we said at the beginning, it’s not us versus them at all. It’s just making sure all sides are heard.ʺ
Is the UK audiology profession fragmented by having different associations giving different messages on the future of hearing care?
Sam Lear: ʺI don’t think there are as much. We have been talking to BSHAA [the British Society of Hearing Aid Audiologists], AIHHP [the Association of Hearing Healthcare Professionals], and the BSA [British Society of Audiology] and meeting with them. And I think essentially we’ve probably got more in common than we have apart, because we’re all the ones with members who are audiologists who are talking about we all really want. Our conversation has kind of led us to a place where all those things that we thought we disagreed on aren’t actually necessarily true, and I think none of us have made any statements that those other bodies essentially disagree with.ʺ
So, is the profession any closer to unifying as one College of Audiology?
Sam Lear: ʺWe’re quite far off that because I think it’s important not to rush into it. We’ve sort of really built up quite a lot of trust, so we’re going to have a collaborative group to work on things and we have suggested things like pathways for referring and signposting and working a bit more holistically together.ʺ
Source: Audiology News UK issue 10 September-October 2024


